COVID-19 Research
Case Report: Positive Outcomes for Second COVID-19 Patient Treated with Laser Therapy
News – 29 September 2020
Dr Scott Sigman today announced the publication of a second case report demonstrating positive outcomes for a COVID-19 patient treated with laser therapy.
Published in the Canadian Journal of Respiratory Therapy, the article describes a remarkable decrease in inflammatory markers, IL-6 and Ferratin, and marked improvement in radiological findings after supportive treatment with Photobiomodulation Therapy (PBMT).1 The patient in this report is part of a randomized clinical pilot trial involving 10 patients with confirmed COVID-19.
Not only did the chest X-ray dramatically clear, but important markers of inflammation, IL-6 and Ferratin, decreased after four days of treatment. Photobiomodulation Therapy is known to have anti-inflammatory effects but in this case, it effectively treated the patient’s respiratory symptoms,” said Dr. Sigman. “As the second patient publication from our trial, hopefully these data will encourage others to consider PBMT as an adjunct treatment option and support additional clinical trials with the use of adjunct PBMT for COVID-19. As we know, there is a continued medical need for safe and effective COVID-19 treatment options.”
The patient, a 32-year-old Asian woman diagnosed with SARS-CoV-2, was treated with once-daily, 28-minute PBMT sessions for four days using an FDA-cleared Multiwave Locked System (MLS) Therapy Laser (ASA Laser, Italy). The MLS Therapy Laser used in this study is distributed exclusively in North America by Cutting Edge Laser Technologies based in Rochester, N.Y. The patient’s response to PBMT was evaluated by comparing different scoring tools before and after laser therapy, all of which improved following therapy. Results showed increased oxygen saturation (from 88–93% to 97%), improved RALE Chest X-ray score (from 8 to 3), and decrease in inflammatory markers: IL-6 levels (45.89 pg/mL to 11.7 pg/mL) CRP levels (3.06 mg/dL to 1.43 mg/dL) and Ferratin levels (359 ng/mL to 175 ng/mL).
Prior to treatment, the patient had shortness of breath and difficulty with activities of daily living. Upon completion of treatment, the patient was able to independently ambulate and greatly improved her ability to perform activities of daily living. Two days following the final treatment, the patient was discharged with minimum supportive oxygen. Two days after being discharged, the patient was weaned to room air.
In PBMT, light is applied over damaged tissues, and light energy is absorbed by cells starting a cascade of molecular reactions that improve cell function and enhance the body’s healing process. PBMT has demonstrated anti-inflammatory effects and is emerging as an alternative modality in pain management, lymphedema treatment, wound healing and musculoskeletal injuries. The utilization of supportive PBMT for COVID-19 is based on the theory that the laser light reaches the lung tissue to relieve inflammation and promote healing. Additionally, PBMT is non-invasive, cost-effective, and has no known adverse effects.
After four days of treatment, the chest X-ray dramatically cleared, and important markers of inflammation, IL-6 and Ferratin decreased. Results showed:
- increased oxygen saturation: from 88–93% to 97%;
- improved RALE Chest X-ray score: from 8 to 3;
- decrease in inflammatory markers: IL-6 levels (45.89 pg/mL to 11.7 pg/mL), CRP levels (3.06 mg/dL to 1.43 mg/dL) and Ferratin levels (359 ng/mL to 175 ng/mL).
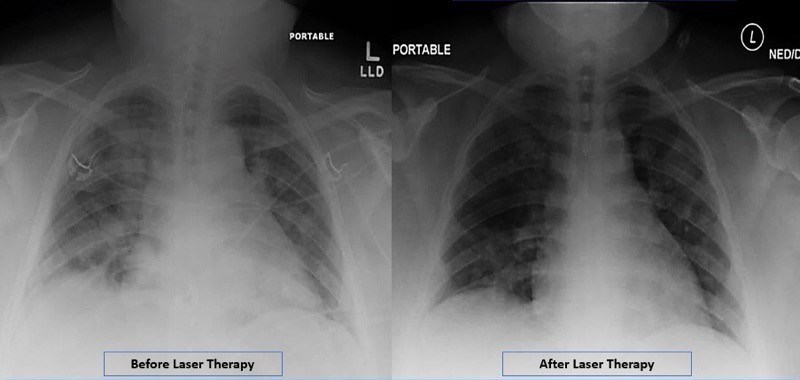 Radiographic Assessment of Lung Edema (RALE) by CXR showed reduced ground-glass opacities and consolidation following PBMT. Lung radiographic score is dependent on extent of involvement based on consolidation or ground-glass opacities for each lung. Total score is the sum of both lungs. RALE score before laser therapy=8. RALE score after laser therapy=3.
Radiographic Assessment of Lung Edema (RALE) by CXR showed reduced ground-glass opacities and consolidation following PBMT. Lung radiographic score is dependent on extent of involvement based on consolidation or ground-glass opacities for each lung. Total score is the sum of both lungs. RALE score before laser therapy=8. RALE score after laser therapy=3.
The MLS laser uses a mobile scanner with 2 synchronized laser diodes, one in pulse mode (adjustable to 1–2000 Hz), emitting at 905 nm, and another in pulsed mode emitting at 808 nm. The two laser wavelengths work simultaneously and are synchronized. The laser is placed 20 cm above the patient across the lung fields while in the prone position. The laser is painless, and patients typically are unaware that the laser treatment is occurring. This laser is routinely used for deeper tissues like hips and pelvic joints that are surrounded by thick muscles. The therapeutic dose used to reach the deep targets of the pelvis is 4.5 J/cm2. Based on calculations by Dr. Soheila Mokmeli, co-author of the study, 7.2 J/cm2 was used over the skin, delivering a therapeutic dose just over 0.01 J/cm2 of laser energy to the lung. This dosage is able to penetrate the chest wall and reach the lung tissue creating an anti-inflammatory effect that in theory blocks the effects of the cytokine storm seen in COVID-19 pneumonia.
